The hidden challenges facing aesthetic medicine professionals in 2026
There's a moment every aesthetic practitioner knows well.
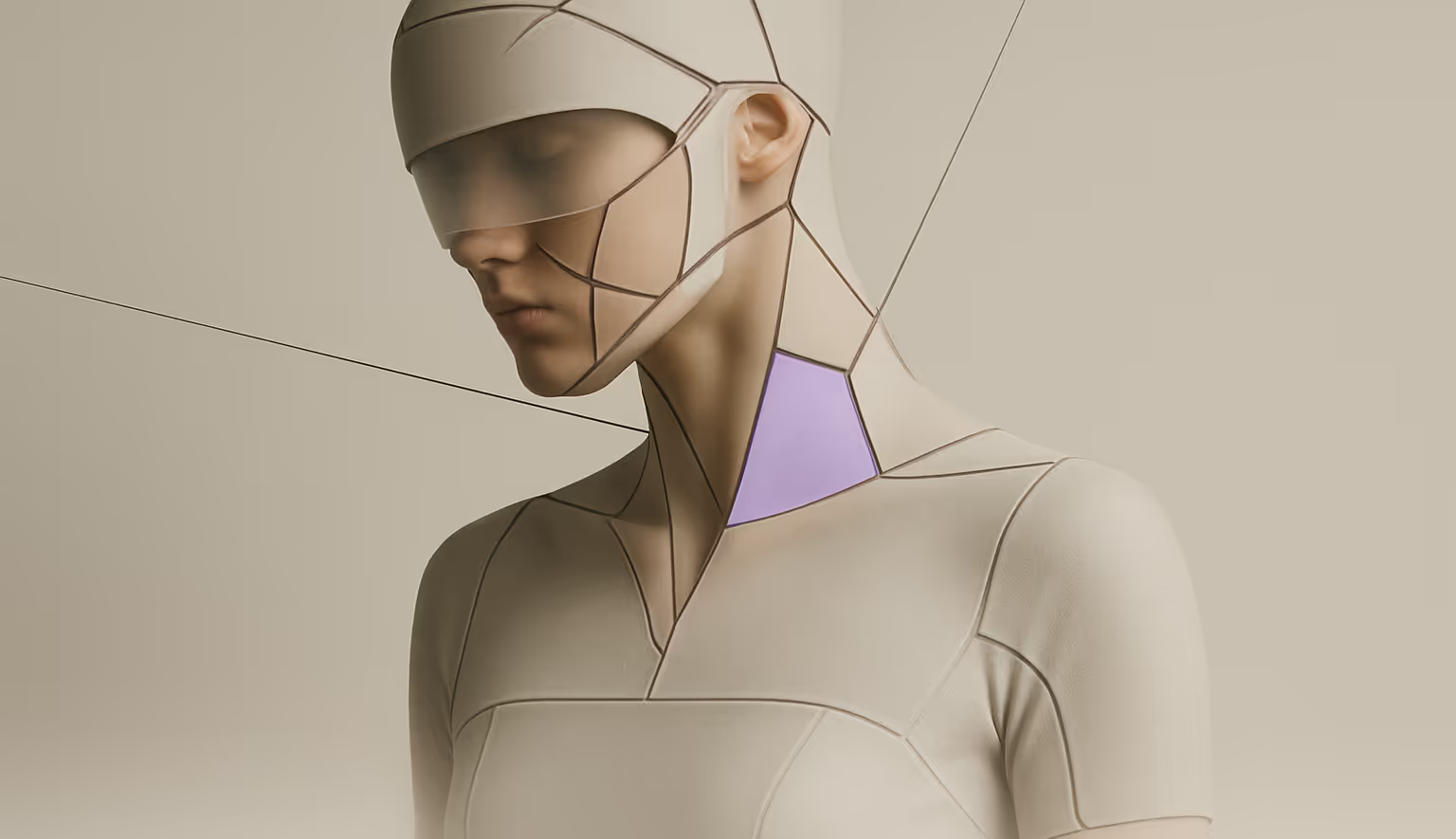
A patient walks in, phone in hand, showing a filtered photo from Instagram. "I want to look like this." The image has been smoothed, lifted, contoured by an algorithm. It doesn't represent what any injection, laser, or scalpel can achieve. It doesn't even represent a real human face.
And yet, somehow, this has become the starting point of the conversation.
A field under pressure
Aesthetic medicine is booming. According to the International Society of Aesthetic Plastic Surgery (ISAPS), nearly 38 million procedures were performed worldwide in 2024 — a 42.5% increase over just four years. The market, valued at roughly $90 billion, is projected to nearly triple by 2033.
These numbers tell a story of extraordinary growth. What they don't reveal is the pressure this growth places on the people delivering care.
Behind every consultation room door, practitioners are navigating something far more complex than technique. They're managing expectations shaped by social media, making judgment calls that balance patient desires against clinical safety, and operating in a field where the boundaries between medicine and consumer service have never been blurrier.
When expectations outpace reality
Here's a statistic that should concern us all: research suggests that approximately 30% of patients arrive with expectations that simply cannot be met safely or anatomically.
This isn't about difficult patients. It's about a cultural shift. Many patients aren't demanding perfection — they're navigating insecurity, comparison, and genuine distress amplified by algorithmic imagery. Social media platforms — Instagram, TikTok, Facebook — have created a visual language of beauty that often clashes with anatomical reality. Filters and editing tools have normalized appearances that no procedure can replicate.
This tension between patient expectations and clinical reality is often reinforced by marketing narratives that move faster than evidence — a dynamic explored in our analysis of the evidence gap between promotion and real-world outcomes in aesthetic medicine.
A systematic review published in 2025 put it plainly: these platforms "promote unrealistic beauty standards and foster exaggerated and often unattainable patient expectations."
For practitioners, this creates a daily ethical tension. Studies consistently find that doctors feel pressured to fulfil requests that conflict with their clinical judgment and safety standards. The patient wants one thing. The practitioner knows what's actually achievable — and safe.
This isn't a minor inconvenience. It's the central challenge of modern aesthetic practice.
The shift to "consumer-driven medicine"
Something fundamental has changed in the doctor-patient relationship within aesthetics.
Traditionally, patients came to physicians with a concern. The doctor assessed, advised, and recommended a course of action. Today, patients increasingly arrive with a specific treatment already in mind — often one they've researched (or think they've researched) online.
This shift toward "consumer-driven medicine" isn't inherently bad. Informed patients can be excellent partners in their own care. But it introduces new pressures.
When a patient views themselves as a consumer purchasing a service, the dynamics change. There's an implicit expectation of delivery. And when that expectation has been shaped by curated social media content rather than medical consultation, the practitioner faces a choice: accommodate a request that may not serve the patient's best interests, or risk the patient walking out — possibly to someone less scrupulous.
The ethical practitioner chooses patient welfare. But that choice has costs, both financial and emotional.
The absence of global standards
Compounding these challenges is a regulatory landscape that hasn't kept pace with the field's growth.
There's no global uniformity in how aesthetic medicine specialists are trained or credentialed. The field sees an increasing number of practitioners from diverse backgrounds — some highly qualified, others less so. Meanwhile, aesthetic procedures are increasingly performed outside traditional medical settings.
For practitioners who have invested years in proper training, this creates frustration. They're competing in a market where credentials aren't always visible to patients, and where social media prominence can be mistaken for clinical expertise.
The irony is sharp: the practitioners most committed to ethical practice often find themselves at a disadvantage against those who promise more, show more, and worry less about what's actually appropriate.
What this means for the field
None of this is intended to paint aesthetic medicine in a negative light. The field serves genuine needs — helping people feel more comfortable in their own skin, restoring confidence after illness or injury, addressing concerns that affect daily life.
But the pressures are real. And they affect practitioners in ways that rarely make it into public conversation.
The research is clear: when practitioners feel caught between market demands and medical ethics, something has to give. Some compromise on their standards. Others burn out. Many simply do their best to navigate an imperfect system, consultation by consultation.
What the field needs — and what patients ultimately benefit from — is a return to fundamentals. Transparent communication. Realistic expectation-setting. Recognition that aesthetic medicine, despite its commercial context, remains medicine.
The best practitioners already know this. They're the ones spending extra time in consultations, gently redirecting unrealistic requests, explaining what procedures can and cannot do. They're prioritising patient welfare over patient volume.
They deserve our support — and patients deserve to be guided to them.
This article is part of iGlowly's ongoing series on challenges and ethics in aesthetic medicine. We believe that transparency — about the field, its pressures, and its standards — serves everyone: practitioners and patients alike.